Keloids are basically masses of overgrown scar tissue. Scarring occurs normally after any
kind of trauma to the skin. But in keloids, this process of scarring gets out of hand and the
body synthesizes excessive scar tissue which is thicker, firmer, and harder than normal scar
tissue.
The word keloid stands for ‘crab-like, named so because the keloidal scar tissue extends
like a crab towards the surrounding normal skin.
Keloid mass consists of thick collagen which is produced by cells called fibroblasts. These
fibroblasts become overactive in certain individuals and cause the formation of keloids. The
main reason for keloid formation is a genetic tendency towards it. Hence, it is seen more
commonly in those who have darker phototypes like type V and VI.
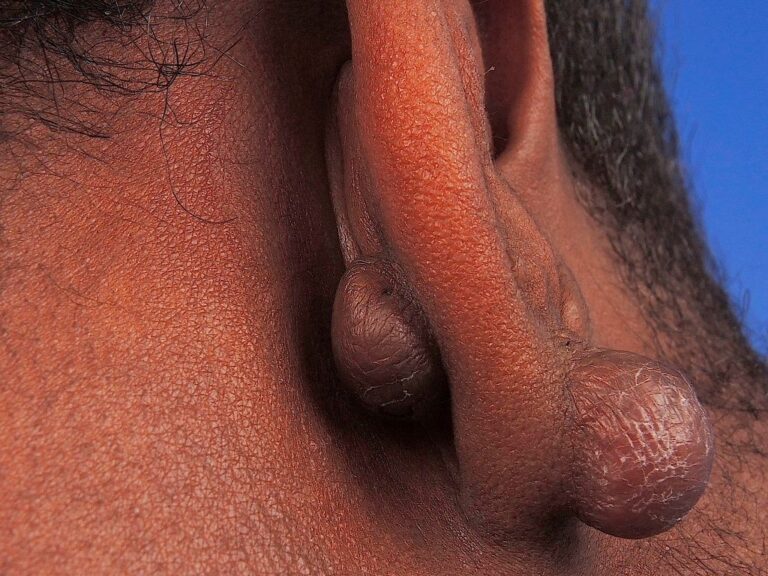
Areas of involvement are the ones where there is maximum tension such as the chest, upper
back, shoulders. Earlobe keloids are also a frequent concern, especially after getting ear
piercings done.
Keloids can occur after:
- Both thermal burns as well as chemical burns (for example, after acid spill)
- Post-surgery at the site of surgical scars
- Minor trauma such as mosquito bites, abrasions, etc
- After acne (especially on the chest and back)
- They can even occur spontaneously, without any trauma
- After any dermatosurgical procedures
Keloid scars are sensitive to sunlight more than normal skin is. They can also get burned
and tanned easily (as compared to normal skin).
Secondly, sun exposure can worsen the appearance of keloids. The contrast between the
surrounding normal skin and the keloid itself can increase making them look worse. It is
important to apply sunscreen over any keloids or scars you may have.
Although they are painless, they can be a source of discomfort for patients by causing
itching and irritation from the growth of the tissue. Sometimes, they may even get infected.
Keloids are not cancerous.
They can sometimes be confused with a hypertrophic scar but hypertrophic scars are
typically more responsive to treatment.
Prevention:
- Avoid aggressive procedures if you have a tendency towards developing keloids
- Always inform your doctor of a history of keloids in you or your family: this can help
them decide which procedures can be safely done and which cannot. - Avoid trauma as far as possible.
Treatment:
Many options exist for tackling keloids.
These include:
- Cryotherapy: This involves freezing the keloid tissue using liquid CO2 at freezing
temperatures. This destroys the tissue, making the keloid shrink in size. - Intralesional injections: These can be either steroids, hyaluronidase, 5-fluorouracil or
a combination of these. These dissolve the thick collagen and also decrease the
formation of new collagen in the keloid. The drawback is that these tend to be painful. - Silicone gel sheets: These are taped tightly over the keloid and cause the keloid to
shrink by exerting a pressure effect on it. These need to be left on for long hours,
including overnight to achieve significant results over a period of at least 3-4 months.
No one treatment works for all individuals. Multiple sessions using multiple types of
treatment are often needed in order to significantly reduce the size and surface irregularity of
keloids. Patience and persistence is key.
Early initiation of treatment when the keloid is small will ensure better and faster results.
Once keloids have grown too big, they are generally difficult to treat.
References:
- Betarbet U, Blalock TW. Keloids: A Review of Etiology, Prevention, and Treatment. J
Clin Aesthet Dermatol. 2020;13(2):33-43. - Ghazawi FM, Zargham R, Gilardino MS, Sasseville D, Jafarian F. Insights into the
Pathophysiology of Hypertrophic Scars and Keloids: How Do They Differ?. Adv Skin
Wound Care. 2018;31(1):582-595. doi:10.1097/01.ASW.0000527576.27489.0f